Research
While these areas represent the core of our current research focus, we enthusiastically welcome new collaborations and fresh ideas that spark innovative, hypothesis-driven science. We are deeply committed to expanding the boundaries of knowledge and accelerating the discovery of novel therapeutic strategies. By fostering a collaborative and intellectually vibrant environment, we aim to catalyze groundbreaking research that advances human health and transforms the future of cardiovascular and cardiometabolic medicine.
Heart Failure
 Heart failure (HF) is a complex clinical syndrome characterized by the heart’s inability to maintain adequate cardiac output to meet the metabolic demands of the body. It remains one of the leading causes of morbidity and mortality worldwide. Traditionally, HF is classified based on alterations in left ventricular ejection fraction, reflecting its diverse etiologies and underlying pathophysiology. Recognizing the clinical heterogeneity of HF, our laboratory has established a suite of preclinical models that faithfully recapitulate the major phenotypes of both heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). These models are developed through induction of ischemic heart disease, a variety of cardiomyopathies, and metabolically driven perturbations that collectively reflect the multifaceted nature of HF pathogenesis. Using these platforms, we investigate the molecular, cellular, and systemic mechanisms that drive HF onset and progression. Our goal is to uncover novel pathophysiological pathways and identify therapeutic targets that can inform the development of effective interventions to prevent, mitigate, or reverse heart failure.
Heart failure (HF) is a complex clinical syndrome characterized by the heart’s inability to maintain adequate cardiac output to meet the metabolic demands of the body. It remains one of the leading causes of morbidity and mortality worldwide. Traditionally, HF is classified based on alterations in left ventricular ejection fraction, reflecting its diverse etiologies and underlying pathophysiology. Recognizing the clinical heterogeneity of HF, our laboratory has established a suite of preclinical models that faithfully recapitulate the major phenotypes of both heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). These models are developed through induction of ischemic heart disease, a variety of cardiomyopathies, and metabolically driven perturbations that collectively reflect the multifaceted nature of HF pathogenesis. Using these platforms, we investigate the molecular, cellular, and systemic mechanisms that drive HF onset and progression. Our goal is to uncover novel pathophysiological pathways and identify therapeutic targets that can inform the development of effective interventions to prevent, mitigate, or reverse heart failure.
Gut-Host Interaction
 The dynamic interplay between the gut microbiome and its host is increasingly recognized as a central regulator of human health and disease. This bidirectional relationship influences a wide array of physiological processes, and its disruption is implicated in the development and progression of numerous chronic conditions, including cardiovascular disease. Modifiable lifestyle factors—such as diet, physical activity, and tobacco use—profoundly shape the composition and function of the gut microbiota. These environmental influences drive shifts in microbial-derived metabolites, many of which possess hormone-like properties capable of modulating host endocrinology, cellular signaling pathways, and systemic homeostasis. Our research focuses on elucidating the mechanistic links between gut-derived metabolites and cardiovascular pathophysiology. We aim to understand how alterations in gut-host interactions contribute to increased susceptibility and severity of cardiovascular disease. By identifying key metabolic and signaling pathways involved in this axis, we seek to develop innovative therapeutic strategies that target the gut microbiome to prevent or attenuate cardiovascular risk and progression.
The dynamic interplay between the gut microbiome and its host is increasingly recognized as a central regulator of human health and disease. This bidirectional relationship influences a wide array of physiological processes, and its disruption is implicated in the development and progression of numerous chronic conditions, including cardiovascular disease. Modifiable lifestyle factors—such as diet, physical activity, and tobacco use—profoundly shape the composition and function of the gut microbiota. These environmental influences drive shifts in microbial-derived metabolites, many of which possess hormone-like properties capable of modulating host endocrinology, cellular signaling pathways, and systemic homeostasis. Our research focuses on elucidating the mechanistic links between gut-derived metabolites and cardiovascular pathophysiology. We aim to understand how alterations in gut-host interactions contribute to increased susceptibility and severity of cardiovascular disease. By identifying key metabolic and signaling pathways involved in this axis, we seek to develop innovative therapeutic strategies that target the gut microbiome to prevent or attenuate cardiovascular risk and progression.
CNS in Cardiometabolic Disease
 There remains a significant gap in our understanding of how sensory inputs from peripheral organs—such as the gut, liver, kidney, and heart—are integrated by the central nervous system (CNS) to produce coordinated, multi-organ physiological responses. This gap is particularly evident in the context of CNS-cardiovascular system interactions. While classical autonomic reflexes, such as the baroreceptor reflex, have been well characterized, far less is known about how more complex and dynamic inputs—especially those influenced by diet and the gut microbiome—modulate central processing and output. Emerging evidence suggests that dietary components (e.g., excessive fats and sugars) and gut microbial dysbiosis can profoundly alter visceral sensory signaling to the CNS. These altered inputs may reinforce maladaptive neural circuits—particularly those involving dopaminergic pathways—contributing to the development and persistence of cardiometabolic comorbidities such as obesity, type 2 diabetes, and hypertension. These conditions, in turn, exacerbate adverse cardiovascular outcomes through a feed-forward cycle of neural and metabolic dysfunction. Our research aims to unravel the mechanisms by which gut microbial reorganization and gut-derived metabolites influence somatosensory and autonomic processing within the CNS, ultimately promoting cardiovascular and cardiometabolic disease (CMD). We are also investigating how emerging therapeutics—both microbiome-targeted and centrally acting—modulate these gut–brain–heart communication pathways, with the goal of identifying novel strategies to interrupt disease progression and restore cardiometabolic homeostasis.
There remains a significant gap in our understanding of how sensory inputs from peripheral organs—such as the gut, liver, kidney, and heart—are integrated by the central nervous system (CNS) to produce coordinated, multi-organ physiological responses. This gap is particularly evident in the context of CNS-cardiovascular system interactions. While classical autonomic reflexes, such as the baroreceptor reflex, have been well characterized, far less is known about how more complex and dynamic inputs—especially those influenced by diet and the gut microbiome—modulate central processing and output. Emerging evidence suggests that dietary components (e.g., excessive fats and sugars) and gut microbial dysbiosis can profoundly alter visceral sensory signaling to the CNS. These altered inputs may reinforce maladaptive neural circuits—particularly those involving dopaminergic pathways—contributing to the development and persistence of cardiometabolic comorbidities such as obesity, type 2 diabetes, and hypertension. These conditions, in turn, exacerbate adverse cardiovascular outcomes through a feed-forward cycle of neural and metabolic dysfunction. Our research aims to unravel the mechanisms by which gut microbial reorganization and gut-derived metabolites influence somatosensory and autonomic processing within the CNS, ultimately promoting cardiovascular and cardiometabolic disease (CMD). We are also investigating how emerging therapeutics—both microbiome-targeted and centrally acting—modulate these gut–brain–heart communication pathways, with the goal of identifying novel strategies to interrupt disease progression and restore cardiometabolic homeostasis.
Metabolic-Associated Steatotic Liver Disease
Metabolic-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease (NAFLD), is a spectrum of liver disorders characterized by the accumulation of fat in the liver in the absence of significant alcohol consumption. MALSD is closely linked to metabolic dysfunction, including obesity, insulin resistance, type 2 diabetes, dyslipidemia, and hypertension, reflecting its systemic nature and association with cardiometabolic risk. The pathogenesis of MASLD is multifactorial, involving complex interactions between altered lipid metabolism, oxidative stress, gut microbiota dysbiosis, and chronic inflammation. Despite its rising global prevalence, there are currently no FDA- 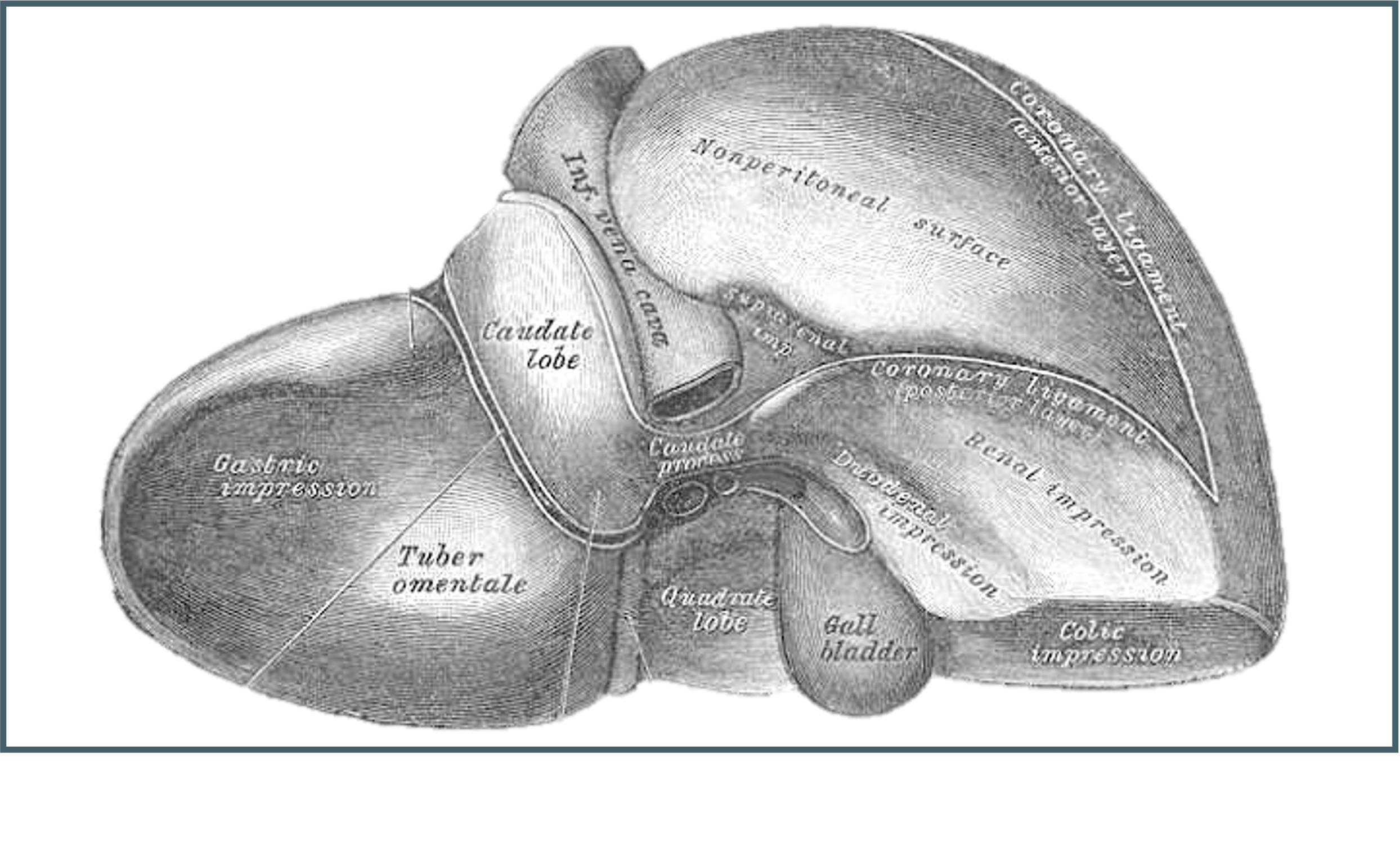 approved pharmacologic treatments, and management primarily focuses on lifestyle interventions targeting weight loss and metabolic control. MASLD also poses significant cardiovascular implications, as it is independently associated with increased risk of atherosclerosis and cardiovascular events—the leading cause of death in affected individuals. As such, MASLD represents a critical intersection between liver health and systemic metabolic disease, underscoring the need for integrated therapeutic strategies and early intervention especially in those who suffer with cardiometabolic disease.
approved pharmacologic treatments, and management primarily focuses on lifestyle interventions targeting weight loss and metabolic control. MASLD also poses significant cardiovascular implications, as it is independently associated with increased risk of atherosclerosis and cardiovascular events—the leading cause of death in affected individuals. As such, MASLD represents a critical intersection between liver health and systemic metabolic disease, underscoring the need for integrated therapeutic strategies and early intervention especially in those who suffer with cardiometabolic disease.
Cardio-Renal Syndrome
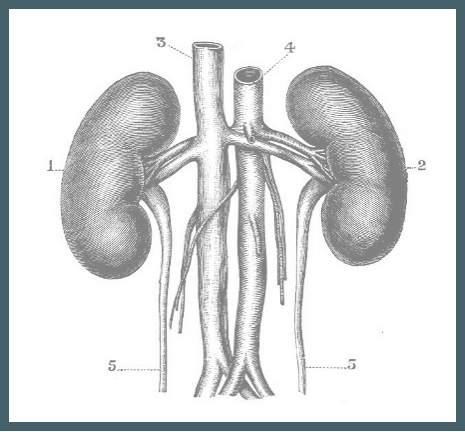 Cardio-renal syndrome (CRS) is a complex, bidirectional disorder in which dysfunction in either the heart or the kidneys leads to progressive impairment of the other organ. This condition underscores the intricate physiological interplay between the cardiovascular and renal systems, driven by shared hemodynamic, neurohormonal, and inflammatory pathways. The pathophysiology of CRS involves a complex interplay of neurohormonal activation—particularly of the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system (SNS)—as well as hemodynamic disturbances, including venous congestion and reduced cardiac output. These are compounded by systemic inflammation, oxidative stress, endothelial dysfunction, and progressive fibrosis in both organs. The management of CRS remains challenging due to the difficulty in treating coexisting heart and kidney failure, and the lack of robust evidence-based therapies tailored to this syndrome. Given its high morbidity and mortality, CRS represents a significant clinical concern, requiring an integrated, multidisciplinary approach to care. We seek to understand the complex interplay through comics-based analysis in models of CRS.
Cardio-renal syndrome (CRS) is a complex, bidirectional disorder in which dysfunction in either the heart or the kidneys leads to progressive impairment of the other organ. This condition underscores the intricate physiological interplay between the cardiovascular and renal systems, driven by shared hemodynamic, neurohormonal, and inflammatory pathways. The pathophysiology of CRS involves a complex interplay of neurohormonal activation—particularly of the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system (SNS)—as well as hemodynamic disturbances, including venous congestion and reduced cardiac output. These are compounded by systemic inflammation, oxidative stress, endothelial dysfunction, and progressive fibrosis in both organs. The management of CRS remains challenging due to the difficulty in treating coexisting heart and kidney failure, and the lack of robust evidence-based therapies tailored to this syndrome. Given its high morbidity and mortality, CRS represents a significant clinical concern, requiring an integrated, multidisciplinary approach to care. We seek to understand the complex interplay through comics-based analysis in models of CRS.
Preclinical Translational Research
 Preclinical research plays a critical role in bridging the gap between basic science and clinical application, offering a translational platform that closely mimics human anatomy, physiology, and disease progression. These models provide greater physiological relevance, particularly in fields like cardiovascular, renal, and metabolic research, where organ size, heart rate, and vascular architecture align more closely with human systems. These models allow for the use of clinical-grade imaging, surgical interventions, catheter-based techniques, and device testing, thereby enabling more accurate assessment of therapeutic efficacy and safety prior to human trials. Moreover, the ability to monitor longitudinal outcomes and perform invasive assessments in real time enhances the mechanistic understanding of disease processes and treatment responses. Despite their higher cost and resource intensity, these studies are invaluable for refining dosing strategies, optimizing delivery methods, and validating biomarkers or endpoints relevant to human disease. As such, we believe this research represents an essential step in the translational pipeline, ensuring that promising preclinical findings are robust, reproducible, and applicable to clinical settings. We have more than a decade of experience in developing and utilizing these preclinical models for interdisciplinary research in CT surgery, cardiovascular disease, gastrointestinal, pulmonary critical care and other fields.
Preclinical research plays a critical role in bridging the gap between basic science and clinical application, offering a translational platform that closely mimics human anatomy, physiology, and disease progression. These models provide greater physiological relevance, particularly in fields like cardiovascular, renal, and metabolic research, where organ size, heart rate, and vascular architecture align more closely with human systems. These models allow for the use of clinical-grade imaging, surgical interventions, catheter-based techniques, and device testing, thereby enabling more accurate assessment of therapeutic efficacy and safety prior to human trials. Moreover, the ability to monitor longitudinal outcomes and perform invasive assessments in real time enhances the mechanistic understanding of disease processes and treatment responses. Despite their higher cost and resource intensity, these studies are invaluable for refining dosing strategies, optimizing delivery methods, and validating biomarkers or endpoints relevant to human disease. As such, we believe this research represents an essential step in the translational pipeline, ensuring that promising preclinical findings are robust, reproducible, and applicable to clinical settings. We have more than a decade of experience in developing and utilizing these preclinical models for interdisciplinary research in CT surgery, cardiovascular disease, gastrointestinal, pulmonary critical care and other fields.
Laboratory Collaborations
Lefer Laboratory - Cedars Sinai Medical Center
Brown Laboratory - Lerner Research Institute, Cleveland Clinic
Makarewich Laboratory - Cincinnati Children's Hospital

